 When I was pregnant with my firstborn I hated being asked my due date. “Spring” was what we would say, which prompted puzzled expressions and sometimes a flurry of questions. However, making it to Spring, to that coveted 32 week mark by which there is a low chance of long-term complications, was less likely for me than the average momma to be. For I had one of many Mullerian anomalies, a uterine septum.
When I was pregnant with my firstborn I hated being asked my due date. “Spring” was what we would say, which prompted puzzled expressions and sometimes a flurry of questions. However, making it to Spring, to that coveted 32 week mark by which there is a low chance of long-term complications, was less likely for me than the average momma to be. For I had one of many Mullerian anomalies, a uterine septum.
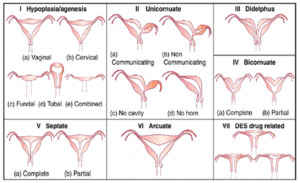
Three to four percent of women in the United States have a Mullerian anomaly, a congenital disorder where the uterus deviates in at least one way from the desired shape for carrying a child. A septum is the most common, and it is a fibrous band of tissue that divides in part or in full the uterus. Many women never know that they have one and others often find out during pregnancy or when seeking fertility treatment, as there is an increased chance of miscarriage.
Living With A High Risk Pregnancy
I learned of my septum when I was six weeks pregnant. I was bleeding and thought I had miscarried. The ultrasound revealed both that my son was still there but that there was a septum. While pregnant it is too hard to see how extensive the septum is, as you can’t do the required tests then. Much of my first pregnancy was a scary waiting game filled with frequent ultrasounds, a lack of information, some misinformation, and hoping for the best. My greatest fear was a baby born between 24-31 weeks, which I knew I had an increased chance of. When I hit the 32 week mark I celebrated!
A Challenging Birth Experience & A Healthy Baby
My water broke at 34 weeks, which was no surprise with my knowledge of the risks. Unfortunately I wasn’t seen immediately once I showed up at the hospital, despite being in active labor with a breech baby and a septum. When I received a physical examination the doctors discovered a cord prolapse, a life-threatening condition that doctors and I believe could be liked with the septum. Less than ten minutes later my baby was in my husband’s arms while I struggled to combat the nausea brought on by the C-section.
 Thankfully my son was never in distress. His heart rate was fine the entire time. I heard “Apgar eight” after his birth and I was so, so happy. Despite being born under five pounds my son surprisingly never went to the NICU, and as I had hoped for my post-32 week babe he has no complications.
Thankfully my son was never in distress. His heart rate was fine the entire time. I heard “Apgar eight” after his birth and I was so, so happy. Despite being born under five pounds my son surprisingly never went to the NICU, and as I had hoped for my post-32 week babe he has no complications.
Hopefulness With A Second Pregnancy
Last year I has my septum resected (aka fully removed, which was done hysteroscopically). I am now pregnant with another child that’s more likely to go to term. There is still fear and lingering trauma, but I’m optimistic that I may get to term, or even closer, this time.
(Many) Frustrations Around My High Risk Pregnancy
I’m so grateful for a healthy little boy, but also very frustrated with the lack of information and the varied medical treatment I received during my first pregnancy and birth. Why can’t we understand the real risks of uterine septums and other uterine abnormalities? Why did different doctors tell me different things about my risks and options? Why did I often rely on being my own researcher and getting my doctor friends to look at my ultrasounds and send me medical journal articles, and why was there such little information to be found overall? And when I was in what I knew was a risky labor and felt it was a dangerous situation, why was I asked to wait rather than given the chance to see a doctor immediately? Our system is broken and our country has a long way to go.
I dream about starting an NGO focused on supporting women with uterine abnormalities so they can have access to information and make better decisions. Yet my wacky and beautiful life with many family and vocational pursuits has me far too busy to take this leap. What I CAN do is leave you with a list of information and wisdom I learned on my journey with a high risk pregnancy and traumatic birth.
My Tips for Surviving a High Risk Pregnancy
- Get the medical journal articles and read them. If you don’t have doctor friends ask your doctor to send you articles that go over the risks and options for any condition you have.
- Go to a smaller practice if you can. I sometimes felt like a number that was lost in the system before. In my new two-doctor practice I feel I’m getting the care I need without having to repeat my story each time.
- Have an advocate and don’t be afraid to push (or have him/her push) if needed. You know your body and if you have reason for concern there’s a good chance it’s valid.
- Educate others, including friends, and have patience with the world. Give a heaping dose of grace when others don’t understand your unique situation and see if you can calmly educate others about how pregnancy can be very different from person to person.
- If you want to have another child, figure out your list of repeats and non-repeats for things that you can control. Also, realize that your first pregnancy issues may or may not be indicative of future ones.
- Who you share with and what you share is up to you.
- Our system may be broken, but you are strong. Mothers are incredibly resilient. If you feel you need therapy, please get it, and use all the support systems you have.
- Be the change you seek. If you so desire, you should feel free to share your story in an effort to educate others. We can also advocate and vote for people who invest in women’s health and supporting mothers during and after pregnancy.
Have you had a complex pregnancy or birth? What tips would you offer moms? Please share them in the comments below!














